Description
Did you know that you need to maintain the insurance company settings in your system?
Insurance companies do not always notify offices when they have made changes to their claims processing to allow for more features, the best way for you to find out is by checking the CDANet carrier list for the companies that you use frequently.
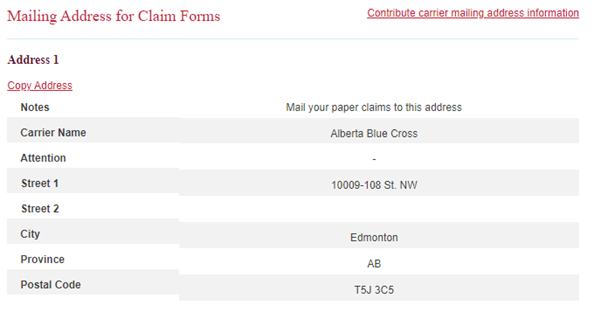
The link below will take you to the CDANet carrier’s list on their website. Each insurance company that accepts electronic claims will be listed here.
https://cda-adc.ca/en/services/cdanet/networks_insurance_new/#/
Click on News to see any news releases done in the past few years. Not all changes will be listed there, but it is a source of information to be referenced.
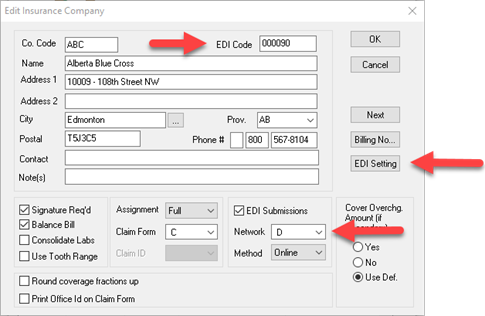
The Carrier ID is the EDI code at the top right corner of the Insurance Company window in Power Practice
Version will be listed as 2 or 4. In Power Practice, Version 2 is equivalent to network N (NDC now known as Telus Group B) Version 4 is network D (NDC Version4).
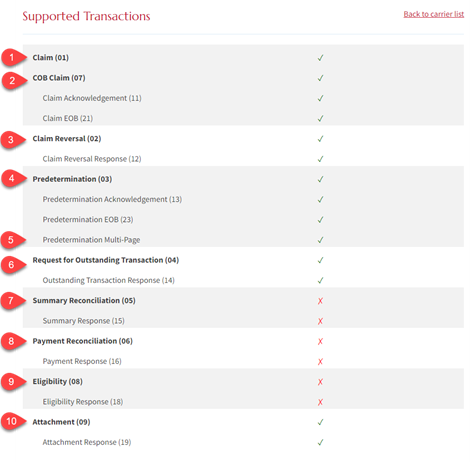
Supported Transaction Types shows a list of items the insurance company can perform electronically.
Note: In Power Practice, if the insurance company is in version 4, the EDI Settings button will be available for you to select the transaction types to match the CDANet list.
Age Limit (Days) shows how many days the company accepts electronic claims for. There is no setting in Power Practice for this, it will attempt to send any claim less than a year old electronically.
How Insurance Company Information is Translated to Power Practice
Read the Supported Transactions section and for each green checkmark, check the corresponding EDI Setting
Note: The EDI Settings for the Insurance Company should match. (Do not check extras)
- Claim
- COB Claim
- Claim Reversal
- Predetermination
- Predetermination Multi-Page – New in 5.1
- Request for Outstanding Transaction
- Summary Reconciliation
- Payment Reconciliation
- Eligibility
- Attachment – New in 5.1
Note: Embedded Transactions does not need to be ticked for Coordination of Benefits to work and at this time should not be ticked
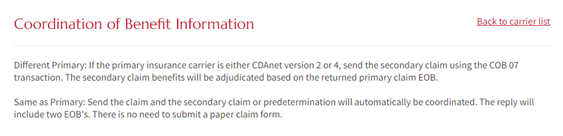
Features used by specific insurance companies
Eligibility – supported by ADSC, Autoben, Beneva, HPEI- Public Health Dental Programs, Quickcard, and TELUS Adjudicare
Multi-Page Predetermination – supported by Alberta BC, Group Health Benefits Solution, Group Source, HPEI- Public Health Dental Programs, Manion Wilkins and Simply Benefits
Attachments – supported by Alberta Blue Cross and Canada Life
Summary and Payment Reconciliation – supported by HPEI- Public Health Dental Programs
What is eligibility and how do I use it with insurance companies that support it?
Eligibility is used to confirm if the patient’s insurance policy information is valid. This feature does not require any treatments to be entered to check eligibility status.
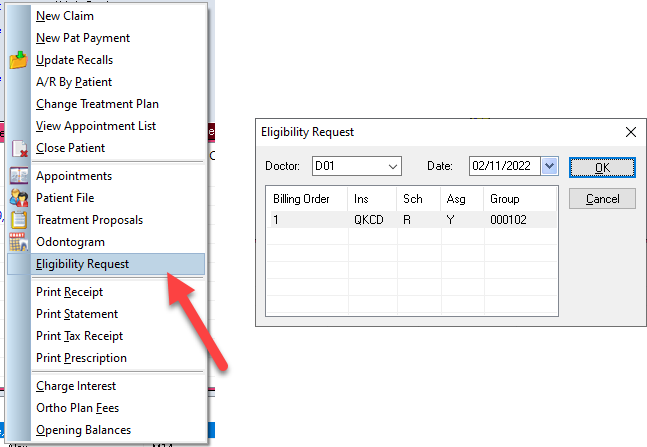
In the Transaction Screen, Right Click in the top portion of the screen (in any tab)
Left click on Eligibility Request in the pop-up menu
Verify the producer and the insurance company you are checking for and click OK
What is payment and summary reconciliation and how do I use with insurance companies that support it?
Payment Reconciliation provides a list of payments from the insurance company which can be used to cross reference payments that have been posted to your office. The summary reconciliation shows all payments posted to your office on that day.
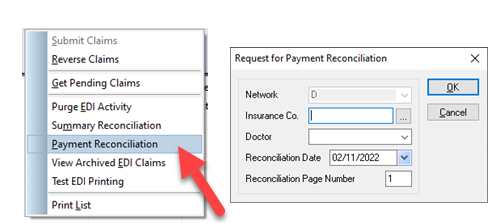
In the EDI Manager, select the Network the insurance company is on and click search
Then right click, then left click on the Summary Reconciliation or the Payment Reconciliation. Pick the Insurance company and the billing doctor desired and click OK