Description
version 5.1+
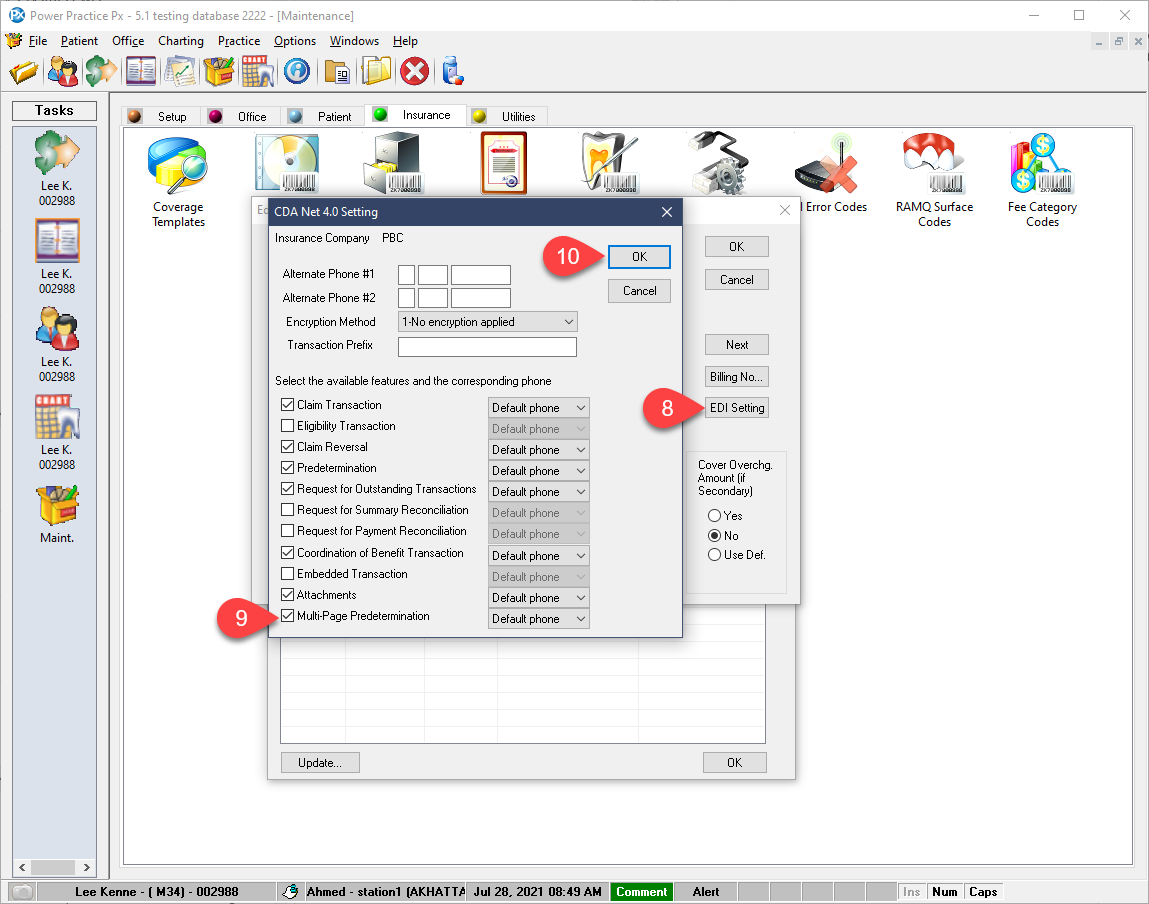
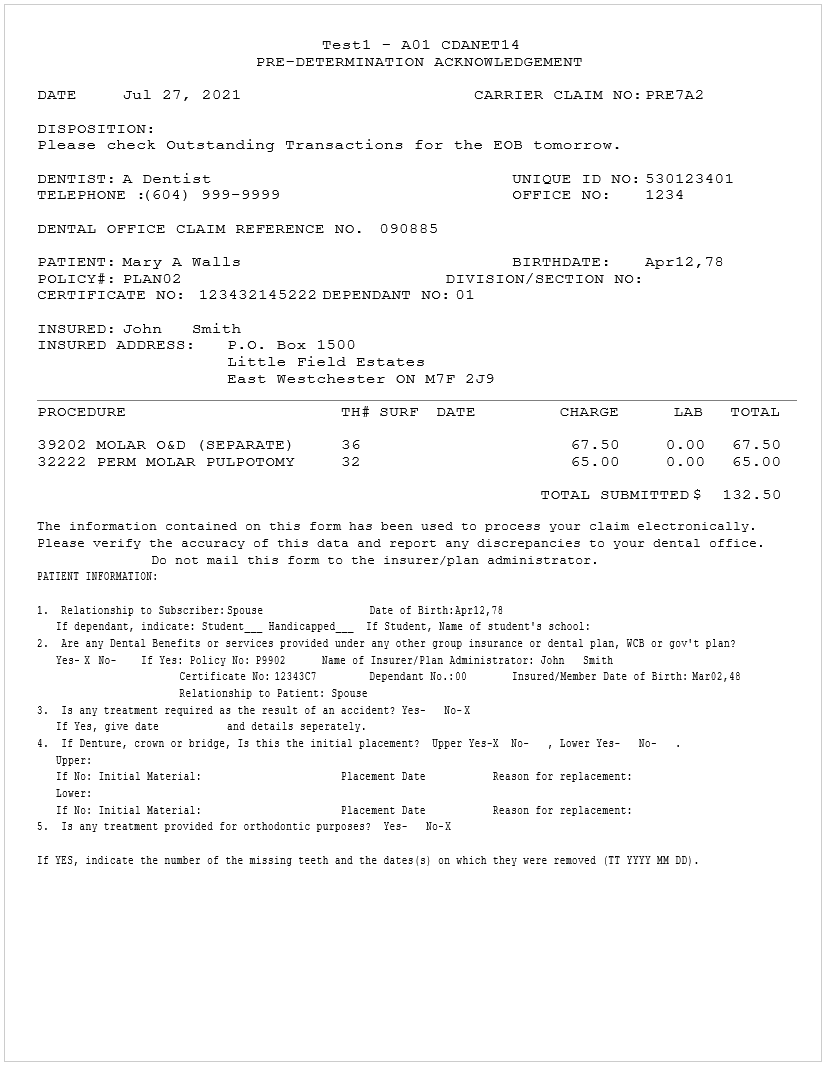
Submissions for pre-approval have previously been limited to seven items per claim. You can now submit your entire treatment plan at once instead of manually breaking it up into separate seven item claims, so long as the insurance company supports the feature.
Notes:
If the patient only has one plan and that carrier allows multi-page predeterminations, the program will not stop you after 7 treatment items.
If primary and secondary both support multi-page submissions, you will also be able to submit more than 7 items at once. However, new claims with the Multipage unticked will behave as normal and limits you to 7.
If only 1 of the 2 carriers accepts multi-page predeterminations, you will still be limited to 7 items per claim, regardless of whether the carriers Coordinate Benefits or not.