Description
version 5.1+
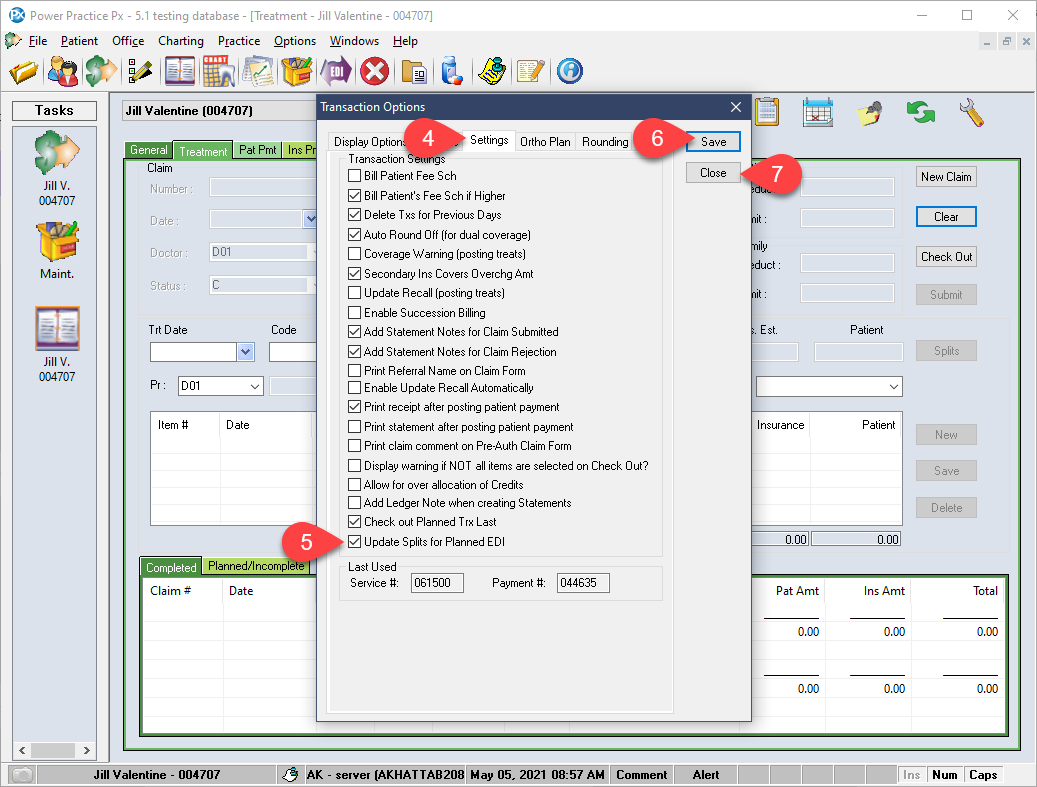
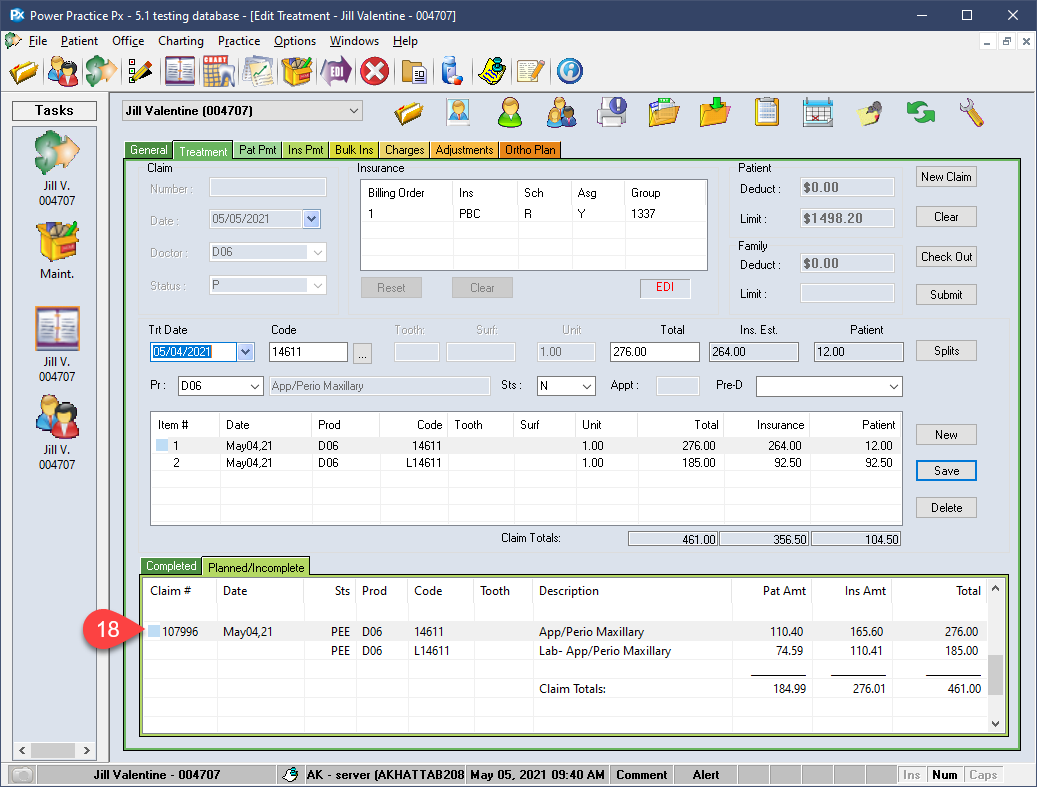
Enable a setting to automatically adjust the patient/insurance fee split for planned treatments. This feature will only affect planned treatments when submitted for pre-authorization and will not take effect for Complete or Incomplete treatments.
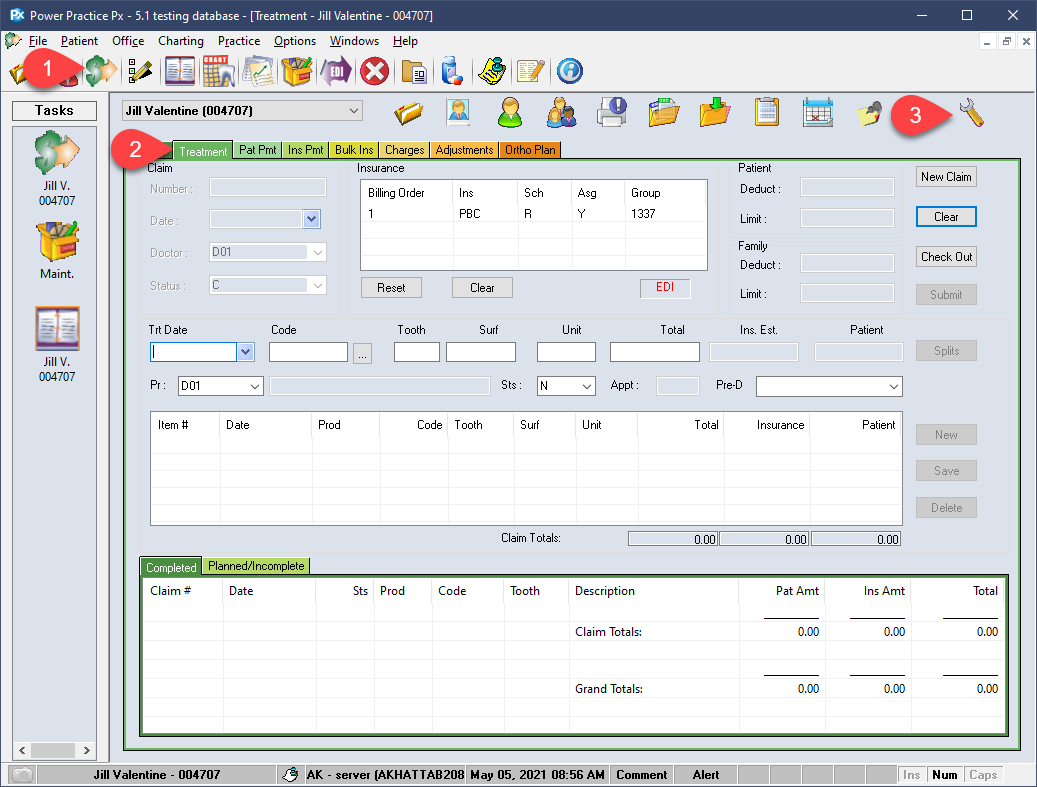
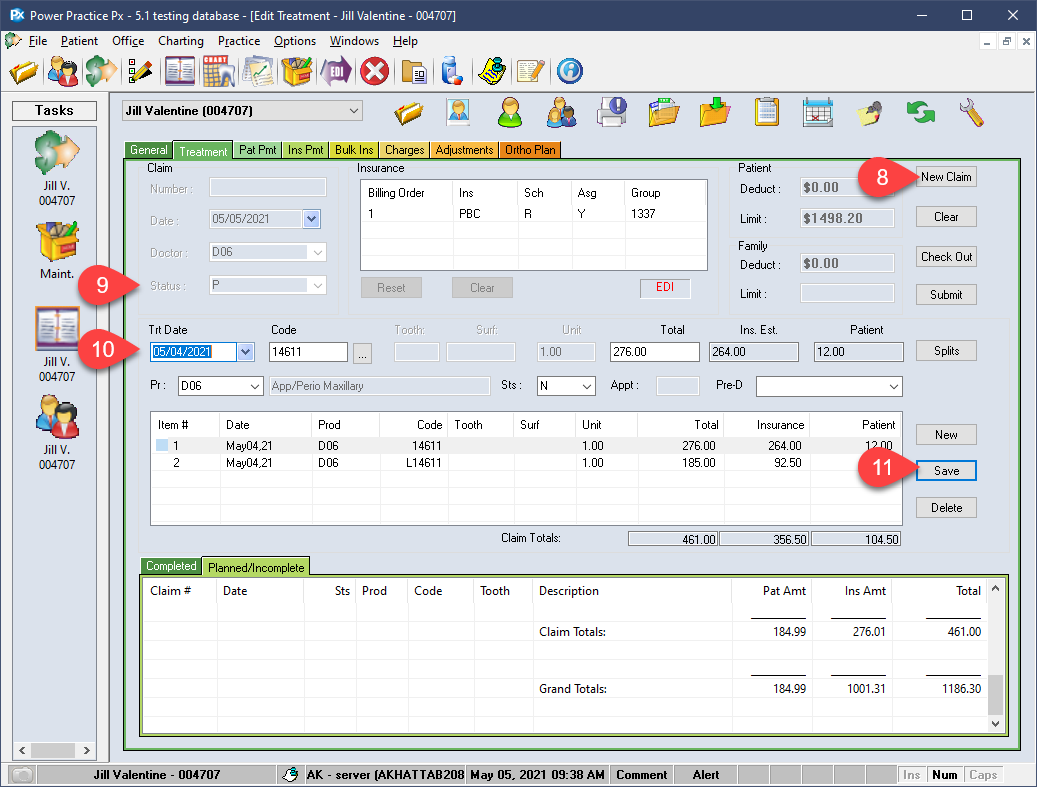
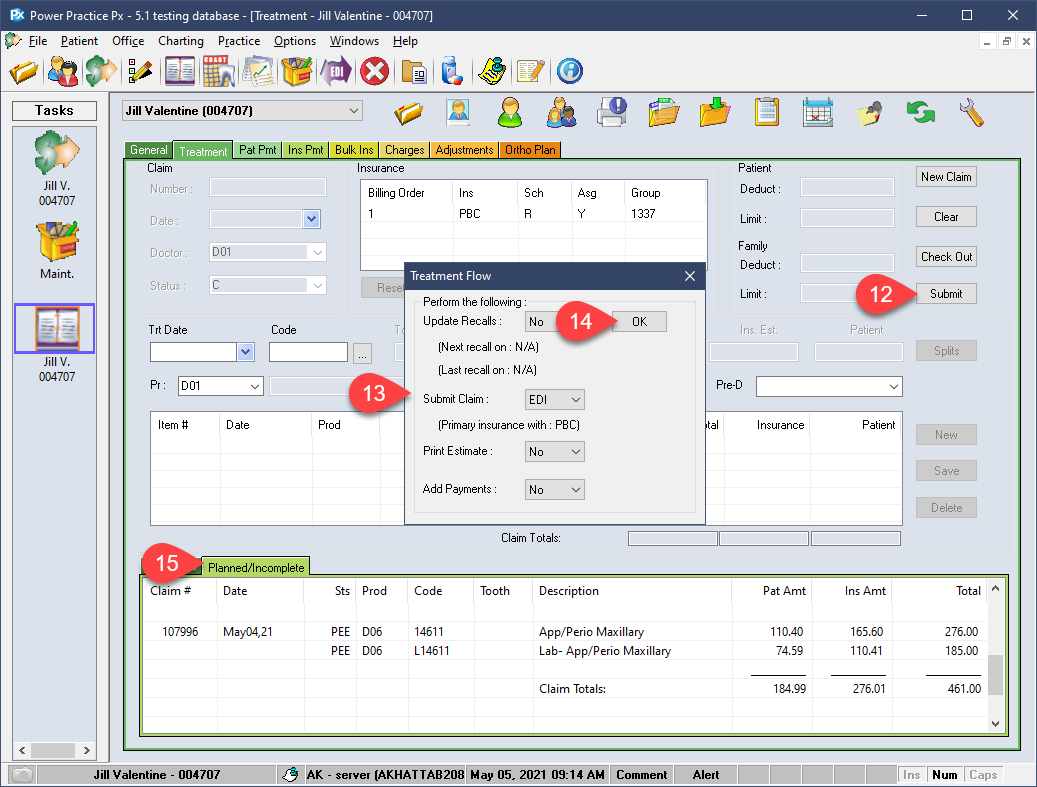
Step-by-Step
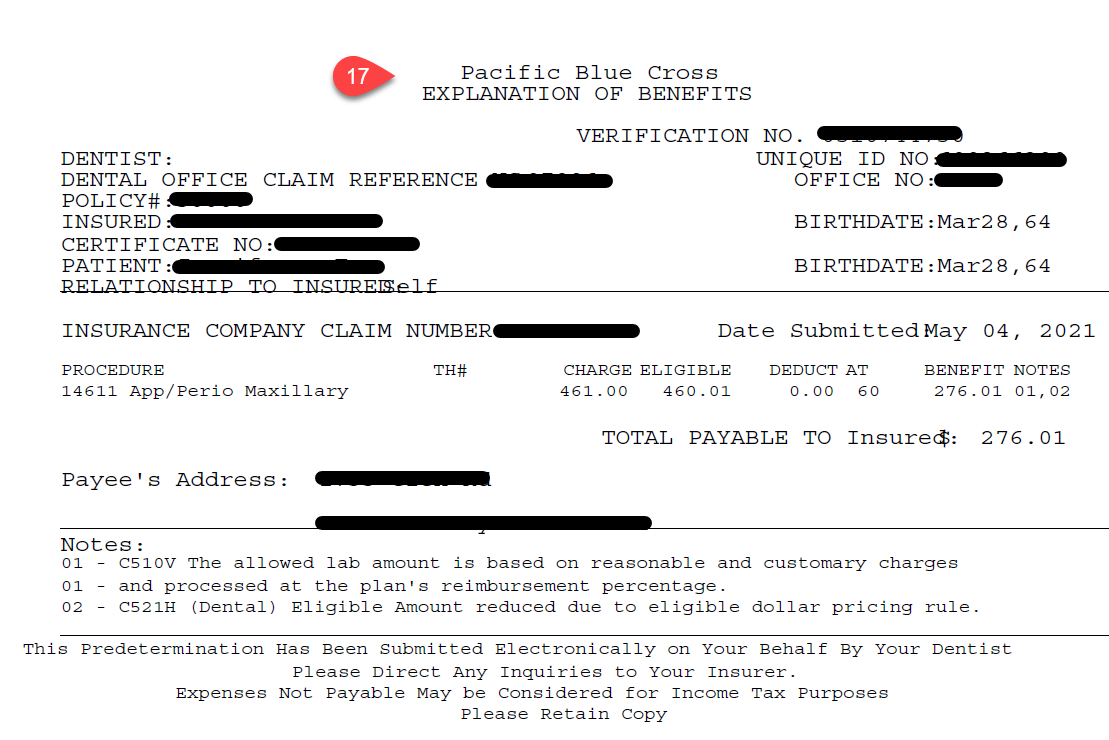
- The information attained via the preauthorization is used by the program to automatically adjust your treatments splits.
You now have all the information required to proceed with your treatment plans confidently. Once the treatment has been delivered to the patient, you can convert the planned items into completed lines, preserving your patient/insurance splits in preparation for payment collection.